AI language models could help diagnose schizophrenia
SOURCE: HTTPS://WWW.SCIENCEDAILY.COM/
OCT 09, 2023
Can AI/ML Help Solve Underrepresentation In Clinical Trials?
SOURCE: CLINICALLEADER.COM
APR 26, 2022
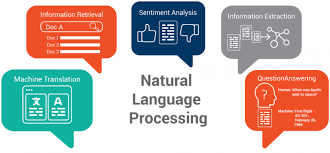
Artificial intelligence (AI) is becoming more commonplace in clinical trials, helping to advance drug development. Forms of AI include natural language processing, graph vectorization, and supervised/unsupervised learning techniques on clinical data to improve and accelerate critical steps in the clinical trials process. For example, AI is used to scan through millions of data points, drawn from published research papers, to predict the absorption, distribution, metabolism, excretion, and toxicity of new drug candidates and hence to find new compounds that can be used in new formulations of medicines.1 AI additionally carries the potential to speed up drug discovery, from what is traditionally several years to several days.
Machine learning (ML) enables powerful inferences to be made from clinical trial data sets and, through learning, the extent of this power increases over time. The more data that is input and the more often errors are corrected, the more reliable the algorithm for future performance. Greater predictive accuracy arises from inputting with heterogeneous data (including suitably representing biological sex). Hence, failing to use representative data or beginning with in-built biases in AI programming becomes a limitation on the seemingly expanding capacity of AI to deliver improved clinical trial outcomes.
To assess medicines for safety and efficacy, it is important that clinical trials are representative of biological sex. Too often, there is an underrepresentation of women in clinical trial subject populations. This leads to erroneous data since women differ in presentation, clinical manifestations, and outcomes in comparison to men.2 For example, many medications metabolize more slowly in women and other medications are more active in men. Clinical manifestations may differ because of the unknown pathophysiology for many disorders, and the drug target identification can differ between the sexes for the same disease. Consequently, since details about clinical trial participants often remains underreported in medical journals, the physician deciding on the optimal treatment for a female patient may not be choosing the most appropriate intervention. Alternatively, the side effects of a medication can be different between men and women.3
Where these biases occur, they undermine the potential that AI presents to translate, scale, and accelerate drug development insights. In addition, if the base algorithm or the training data for an ML model contains some form of bias, it is extremely likely that the resulting models will perpetuate that bias when recommending subject data sets and for interpreting trial data sets.
While women remain underrepresented in too many clinical trials or trials are incorrectly assessed when accounting for female patients, AI presents solutions to these design challenges. For example:
AI-based algorithms are additionally being developed to efficiently probe the pathways of synthesis for novel drug candidates (where there are between-sex differences in terms of genomics information, biochemical attributes, and target tractability exist). To aid researchers, AI can be programmed to respond to verbal questions and requests in the laboratory setting.7 Such processes can help researchers to understand bias and the risks that stem from this and to simultaneously teach the AI to disentangle male-female drug interaction differences.
AI has the power to ensure clinical trials are unbiased from the outset and draw better inferences about the different responses between men and women from clinical trials. This presupposes that the AI is not in itself biased as a result of its programming or learning, and developers need to be mindful of this possibility.
References
About The Author:

Tim Sandle, Ph.D., is a pharmaceutical professional with wide experience in microbiology and quality assurance. He is the author of more than 30 books relating to pharmaceuticals, healthcare, and life sciences, as well as over 170 peer-reviewed papers and some 500 technical articles. Sandle has presented at over 200 events and he currently works at Bio Products Laboratory Ltd. (BPL), and he is a visiting professor at the University of Manchester and University College London, as well as a consultant to the pharmaceutical industry. Visit his microbiology website at https://www.pharmamicroresources.com.
LATEST NEWS
WHAT'S TRENDING


Data Science
5 Imaginative Data Science Projects That Can Make Your Portfolio Stand Out
OCT 05, 2022

SOURCE: HTTPS://WWW.SCIENCEDAILY.COM/
OCT 09, 2023
SOURCE: HTTPS://WWW.THEROBOTREPORT.COM/
SEP 30, 2023
SOURCE: HTTPS://WWW.SCIENCEDAILY.COM/
AUG 08, 2023
SOURCE: HOUSTON.INNOVATIONMAP.COM
OCT 03, 2022
SOURCE: MEDCITYNEWS.COM
OCT 06, 2022